Big emotions before some big news
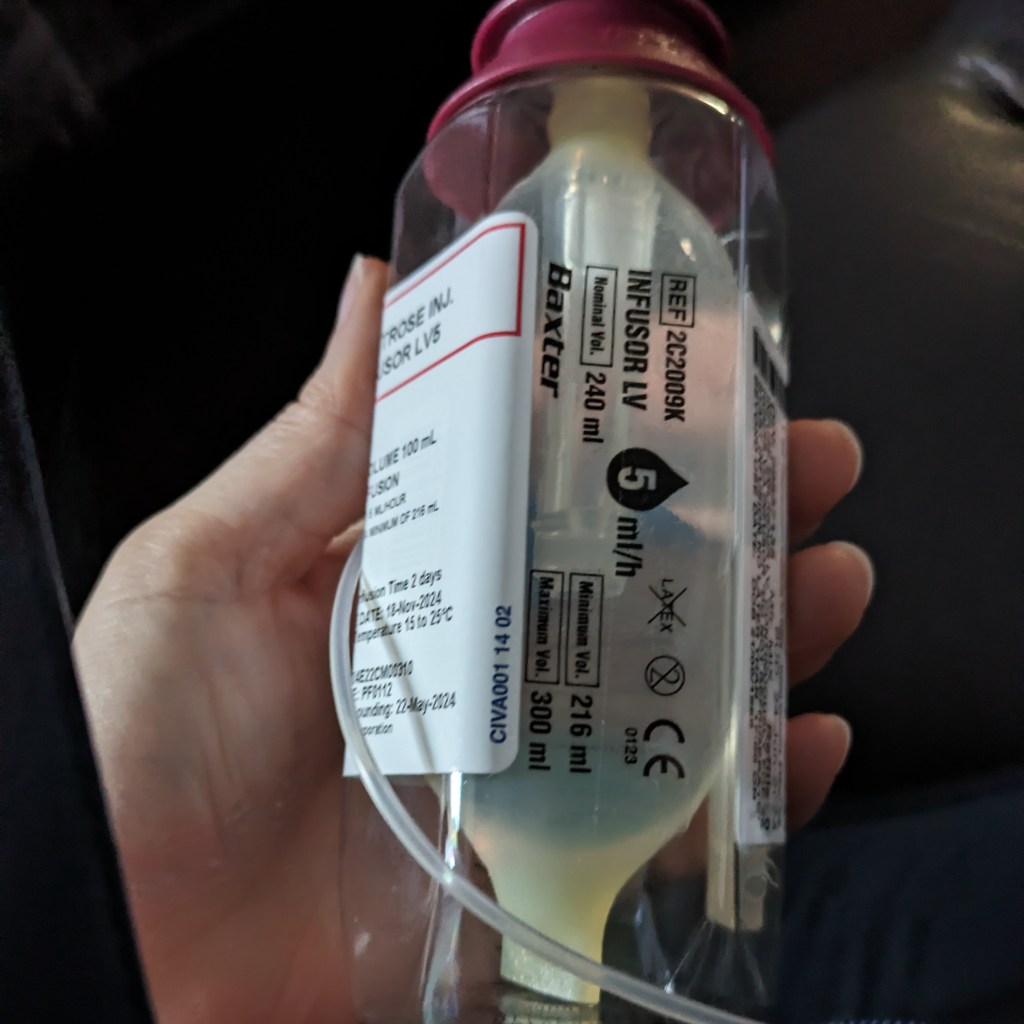
As you may know, I was diagnosed with rectal cancer in February of this year. Due to metastasis to a nearby lymph node it was assessed as stage 3. I did 28 radiation treatments between April 18 and May 28. I started bi-weekly chemo treatments on June 24, ending October 17, for a total of about 400 hours of chemo.
Since October 24, when the chemo-related Grastofil injections ended, I have been in a bit of a state of limbo waiting to find out how well those treatments worked – or not.
This is the week I will find all that out. By Thursday I will know.
So this is a pretty emotional week. It’s been an emotional few weeks leading up to it, to be honest. I even hesitated about writing this post because of all of the emotions going on right now.
Before we get into the meat of things, and you get all worried, let me assure you that while things are pretty heavy right now, they are not always that way.
I’m generally a pretty happy and positive person, even throughout the quagmire that cancer treatments can be. I love to laugh and have fun. At the same time, cancer is some serious shiznit and it’s not always possible to be in a bluebirds-and-rainbows state of mind these days. Shoot…even in regular, every day life, being perpetually happy is not very realistic.
Not to say that I’m in a negative state of mind right now, but I am feeling a lot of things and it really does feel quite heavy.
Helping you help me
If you feel like you want to add a comment or send a text or email to say something supportive, that would be lovely! If you aren’t sure what to say (which is normal), let me help you with that!
The kind of thing I have learned that helps me most is along the lines of “That sucks…that’s a lot to deal with…I wish you didn’t have to go through all this…etc.” It might go against your instincts, but it really does help. 🙂
It turns out that the normal positive platitudes that we all tend to lean towards, such as “You can beat this! You’ll do great! Everything will be fine!”, don’t actually help me. They make me feel worse.
I respect, though, that those types of sayings may be helpful to other folks, so I’m not saying that they aren’t ever appropriate in these situations. Personal journeys are just that – personal and therefore individual so what works for one doesn’t necessarily work for another.
There…That’s done…on we go!
The waiting phase
As I said, I fully completed all my scheduled treatments on October 24 (the end of the Grastofil injections). Since then I’ve been in this waiting-for-results phase.
Annnnnnnnnnnnd…I have learned I am not great at waiting. I was great at the doing – it wasn’t fun and, in different ways and at different times, it was quite difficult and painful, but because I was “doing”, I was mostly OK – not too stressed out, at any rate. I had things to do and side effects to deal with, so I was distracted enough not to be thinking about what would come next. But this whole “nothing left to do but to wait” business is definitely not my forté.
I actually started to feel the stress and pressure of this waiting period two or three weeks before chemo ended. I knew I would need some help navigating this stage so I set up an appointment with my oncology social worker, who had been helpful in earlier stages, before the stress became too heavy.
I keep saying that it’s the waiting phase that is stressing me out. But really, it’s what’s at the end of the waiting that is truly stressful: the results.
These results will tell me if everything worked or if it didn’t and what that means now:
- Will surgery be required?
- If so, what are the options?
- Will a permanent colostomy be required?
- What’s my overall prognosis?
- Am I likely to be part of the 75% of those who do this treatment protocol and get to live another 5 years – or (dare to dream) even longer?
- Or will I be part of the other 25%?
Either way, the emotions come, sometimes one at a time and sometimes in a jumble, and they are all big: hope, fear, worry, gratitude, despair, loneliness, joy…you name it! There’s a big ol’ pot of emotion soup running through my brain and body right now. I feel scared and even terrified one minute and then flip to hopeful and grateful two minutes later before flopping back to scared again. How I haven’t stroked out yet is beyond me!
I’ve been reading Eckhart Tollë’s The Power of Now, but I am definitely not at a point where I can just impassively and neutrally watch emotions come and go. I’m on the roller coaster of emotions more that I probably have ever been in my whole life.
Suffice to say…It’s a lot.
My anchor: Realism combined with hope
In case you don’t know me, I’m not usually one to intentionally borrow trouble. Sufficient is the day and all that. However, these are genuinely huge life impacting questions, so it’s tough to completely avoid thinking about them and what it could all mean for my future. Consequently, it’s very difficult to keep the emotions in check and stable, too.
As with everything else in this journey, I’m not trying to be either optimistic or pessimistic. Instead, I’m shooting for a balanced realism. It is possible that the radiation/chemo got rid of the cancer and it is also possible that they didn’t.
If they did – great! It will still mean very close monitoring (every 2 to 3 months) for the next few years, but it will have bought me some time. If not – well, my day-to-day life will very likely change drastically. Both of those options are very possible outcomes this week.
I am hopeful that it’s the best-case scenario and at the same time, I’m also trying to prepare myself for other alternatives.
How I am coping with it
I have already written a few posts on how I cope with the mental challenges so I won’t go into all those details again here. To give you easy access to potentially helpful ideas, I will link those previous posts below. Here I will just share some things that come to mind now.
As I’ve said in previous posts, I really work to not let the periods of fear, anxiety, and sadness take up permanent residence inside my head. I know from my experiences with depression and anxiety that those two would happily become forever roommates, without even the decency of paying rent, so I consciously work to keep from falling into that kind of cycle.
The further into it you fall, the harder it is to get out, so while I allow myself a certain amount of time to feel what I feel, I also don’t let myself stay in it for too long.
To get out of it, I frequently give myself a task that needs to be done – laundry, organizing a closet, working on a craft, etc. – to get myself out of my head and distracted from those emotions. Watching TV has even helped! The Derry Girls (Netflix) and The Taskmaster (YouTube) have dragged me out of so many moments of sadness with full-on uproarious laughter that I can’t count them. Laughter really does help.
Keeping in touch with the social worker has also been helpful. I can be totally frank with her. She’s an objective third party so I don’t have to worry about worrying her, like I do with friends and family. As a professional, she also has different ideas for coping with things than those in my personal circle would have, which has been very helpful.
Another big help is my personal village of supportive people, as the example below shows. I have also learned how important it is to recognize what I need and to let people know what those needs are, such as earlier when I let you know what type of written or verbal encouragement is most helpful to me, as well as what doesn’t help. Thankfully, because my village of supportive folks is amazing, people have been very receptive and respectful of that.
The gift of a few short words
As an example, my sister-in-law, Mariette, asked me on Monday how I was feeling about the upcoming appointment, if I was worried. I hesitated and finally said yes, I was.
I explained that I probably wouldn’t be as worried if not for the presence of blood every day for the past 4 weeks, which is generally not a good sign, but I’ve let the doctors and nurses know, which is all I can do about that right now. I’m trying not to make a big deal out of it, but that said, I am still worried.
Then she said, “That’s understandable. It’s a big thing.”
If I could have crawled through the phone to hug her at that moment, I would have. That was one of the kindest, sweetest things anybody could have said to me at that moment.
Her simple statements told me, “You are safe in telling me how you really feel. I know this is a very difficult time for you and that you are struggling. These are serious issues you are dealing with, and it’s OK for you to be worried. In fact, it’s natural for you to be worried. I am here for you.”
Her acknowledging the legitimacy of how I felt made me feel stronger and more positive, whereas had she tried something more overtly positive, from the cliché universe, it would have made me feel worse.
I am very grateful to have her as part of my village.
It’s OK to be worried
And she was right. It’s OK that I am worried. I don’t know what the next few days will bring and what decisions I will need to make.
It’s also OK if you are worried for me. I’m the one with cancer, but if you are in my circle, you are going through your own experience with this, too. I hope you have someone in your life to whom you can turn with your concerns and worries about it.
It’s important to be able to talk about it – to just kind of vomit it all out there. Probably not to me, though… To be honest, I don’t know that I’m strong enough to carry me and you through it. I’d probably be fairly useless. But I do know it’s hard on more people than just me. It sucks for you, too. It’s hard to see someone you care about go through something like this.
An imaginary holiday and a life lesson
If I had my druthers, we wouldn’t have to deal with it. Maybe we’d be on a holiday instead. One where a shredded immune system and peripheral neuropathy and tests and scopes and scans are completely unheard of and unnecessary. One where we sit back and relax, enjoying good food, beautiful views, and great company. And lots of laughter.
Maybe one of us forgets to pack the printed tickets for a remote excursion we were looking forward to. There’s no wi-fi and, with no way to access the digital tickets, there’s no excursion for us! Not to be completely thwarted in our wont for adventure, though, we laugh it off and make up our own itinerary for the day – discovering paths and places we never would have if not for the tickets snafu.
Not unlike reality, really. Life often takes us off the paths we have planned and, depending on the attitude we choose to bring to them, those new paths provide experiences, learning, and growth that couldn’t have come any other way.
I assure you cancer was not a path I had on my planned life itinerary. I’ve learned things these past months, though, that I never would or could have otherwise. I’m not glad I have cancer, but I am grateful for the learning and growth I have experienced as a result.
So, while I am worried about what this week will bring, at the same time, I know that whatever unexpected path I end up on, there will be opportunities for more growth and learning there, too. In fact, a part of me is even curious as to how I will meet those challenges, as well as the growth and change I will experience as a result, strange as that may be.
Documenting the moment as we live it
The fact that I know change is on the horizon is one of the reasons I really felt the need to write now – before the waiting ends and before I know whatever it is that is waiting to be known.
Weird as it may sound, I wanted to write about this time with my “while waiting” eyes, rather than with retrospective eyes, which always add different nuances to memories. It wouldn’t be as authentic. And, ultimately, at the end of whatever comes next, I won’t be the same so, I suppose, I wanted to document and give space to the current me.
Does that make any sense? Do you ever feel that way? Something momentous is about to happen and you wonder how you’ll deal with it or where it will take you, conscious that you won’t be the same as a result of it? Maybe it’s just me on a weird tangent. 😀
Sharing what you have learned
Since there is no one approach for support or dealing with life’s challenges, I’d love to hear about your experiences – things that have helped you along your various paths and journeys in life.
- What types of support approaches have helped you?
- How have you let people know what you needed? How was that received?
- How did you prepare to face the unknown?
Please feel free to share your thoughts and experiences in the comments – we can all learn from and help each other!
NOTE: This doesn’t just have to relate to cancer or even just to health issues in general. Things you have learned from other life challenges could be helpful, too. 🙂
More info on mental health struggles
As I mentioned earlier, here are the links to some previous posts where I talked about the mental health challenges I have gone through and things that have helped me. Feel free to share in the comments any resources (websites, reading, etc.) that you have found particularly helpful, too.
- The mental side of things: My journey with cancer (Part 3)
- More on the mental challenges – My journey with cancer (Part 4)
- How I cope: My journey with cancer (Part 7)
Thank you for taking the time to read along and for sharing any of your experiences. I really appreciate it. Building a supportive community, even an online one, can be really helpful. It takes a village to do more than raise a child!
Lucy
If you enjoyed this post and would like to read more, don’t forget to follow!